In the past few months, amid the coronavirus outbreak, life has become drastically different for all of us. Many of us have adjusted to staying in our homes, spending much more time than we’re used to with our families, or by ourselves.
While the stay-at-home orders being issued across the world may be stressful, they have also allowed us to get creative in the ways we connect with our friends and family, and how we work and communicate with colleagues. As the Spatial Biology Company™, we try to stay social while practicing “spatial” distancing. We’ve been sharing baking recipes, pictures of pets (who are very pleased to have their humans home all day!), and even arts and crafts to stave off the boredom.



Some of the ways Akoyans are spending their time at home.
In the scientific community, we’ve seen an amazing outpouring of research from scientists leading the charge in the fight against coronavirus. And it’s not slowing down.
High-dimensional immune profiling is a cause close to our heart because of the work we’ve done in recent years in the field of immunotherapy and immunology – and many of these principles can be extended to infectious disease research. More comprehensive research is needed to understand the impact of the virus on the lungs and immune system and how it can impact screening, diagnosis, and vaccine development. We look forward to supporting researchers in their efforts to understand this virus.
We’ve developed the Phenoptics™ and CODEX® platforms to image biomarkers in tissue samples, but we’ve also recently tested our CODEX platform to profile cell suspensions. We’re hosting a webinar on April 24th to educate our users on using CODEX with PBMCs – you can register here (more details at the end of this post)
In the meantime, here are just a few of the research papers and news stories surrounding COVID-19 that have caught our attention:
1. Predicting disease outcomes from immune response
Researchers from the Peter Doherty Institute for Infection and Immunity profiled the immune response of a patient with a symptomatic, but non-severe case of COVID-19 to understand the breadth and kinetics of that response. They observed recruitment of certain immune cell populations including antibody-secreting cells (ASCs), follicular helper T cells (TFH), and activated CD4+ and CD8+ cells, along with IgM and IgG SARS-CoV-2-binding antibodies in the blood before symptoms resolved.
By characterizing the immune response (and extending that characterization to larger patient cohorts), we may be able to predict disease outcomes early on and identify people at risk for more severe symptoms.
2. Herd immunity and “immunity certificates”
When most of the population develops immunity to a virus, we begin to see the spread of that virus slow down or even stop completely. People develop immunity through vaccines or by contracting the infection and recovering. Vulnerable populations, like the elderly, infants, and those with compromised immune systems, rely on herd immunity to avoid catching the virus themselves. Germany is considering issuing “immunity certificates” to its residents. Using serological tests, they would be able to identify those who recovered from COVID-19 and possibly ease lockdown restrictions in areas that had built up herd immunity.
3. Coronavirus serology test
These immunity certificates might be in the cards for the US as well. The US FDA recently approved a serological test for COVID-19. This test examines the body’s immune response to COVID-19 rather than looking for signs of the actual virus itself. Developed by Cellex Inc., the test would be able to identify any past coronavirus infections. However, since antibodies can take time to develop, it may be less effective at identifying current infection.
The CDC announced that it will begin using this test to determine the number of people who have been infected, including the asymptomatic. Those who have developed antibodies could potentially be allowed to return to work and face fewer restrictions about leaving home.
4. “Peacekeeping” cells fight COVID-19
Kamal Khanna, from NYU Langone Health, and his collaborators have identified a sub-population of macrophages in the lungs, called nerve-and-airway-associated macrophages (NAMs). Instead of consuming pathogens like alveolar macrophages (AMs), they suppress inflammation. AMs and NAMs work together to fight infection and prevent tissue damage.
Because lung inflammation plays a major role in COVID-19, understanding how NAMs regulate inflammation could be helpful in developing therapies for the disease. In NAM-depleted mice, Khanna’s team found higher levels of inflammatory cytokines, including IL-6, which has been observed at elevated levels in people who died from COVID-19, compared to survivors.
5. SARS-CoV-2 and the nervous system
Some patients with COVID-19 have noticed a loss of smell and taste as one of their symptoms. One explanation for this is inflammation at those sites, caused by the immune response. However, a review published earlier this year by Yan-Chao Li from Jilin University and collaborators suggests that SARS-CoV-2 may be able to infiltrate the central nervous system (CNS), causing neurological damage and potentially contributing to the acute respiratory failure seen in patients. Loss of smell and taste could thus be symptoms of this type of attack.
SARS-CoV-2 enters cells through the ACE2 receptor, expressed in multiple cell types, including brain tissue. The virus could attack the CNS through endothelial cells lining blood capillaries in the brain. It could also infect cells innervating the lungs, which might contribute to difficulty breathing. Autopsies of patients who died from COVID-19 could illuminate the role of nervous system damage in disease outcomes.
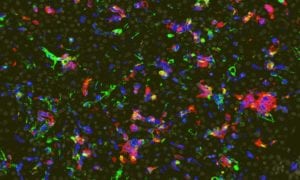
6. Stanford lab studying COVID-19 tissue samples with CODEX
We were honored to hear that Dr. Garry Nolan and his team at Stanford, where CODEX was developed, will begin performing deep immune profiling (using CODEX) on tissue samples from COVID-19 patients. Their goal is to identify immune markers and spatial features associated with disease outcomes. We look forward to seeing the results from their study and how those insights can benefit the scientific community.
If you’re using the CODEX or Phenoptics platforms in your COVID-19 research and need support, please feel to reach out to us. We’re here to offer technical expertise, troubleshooting, help developing panels, and more. Send us an email at support@akoyabio.com.
Our heartfelt thanks to all scientists working tirelessly to improve our understanding of this virus. If you’re interested in learning how to use CODEX with cell suspensions, join us for our webinar on the 24th. We hope you stay safe and healthy!
Webinar | Deep Immune Profiling of Peripheral Blood Mononuclear Cells (PBMCs) with the CODEX® Platform
Friday, April 24th | 9:00 AM PDT
In this webinar, you will learn:
- How the Cell Sciences Imaging Facility at Stanford uses CODEX for deep immune profiling of tissue samples and cell suspensions
- How the CODEX Multiplex Analysis Viewer (MAV) can be used for gating and clustering different cell populations
- Why the CODEX Benchtop Solution is a simple, cost-effective workflow for deep immune profiling of cell suspensions